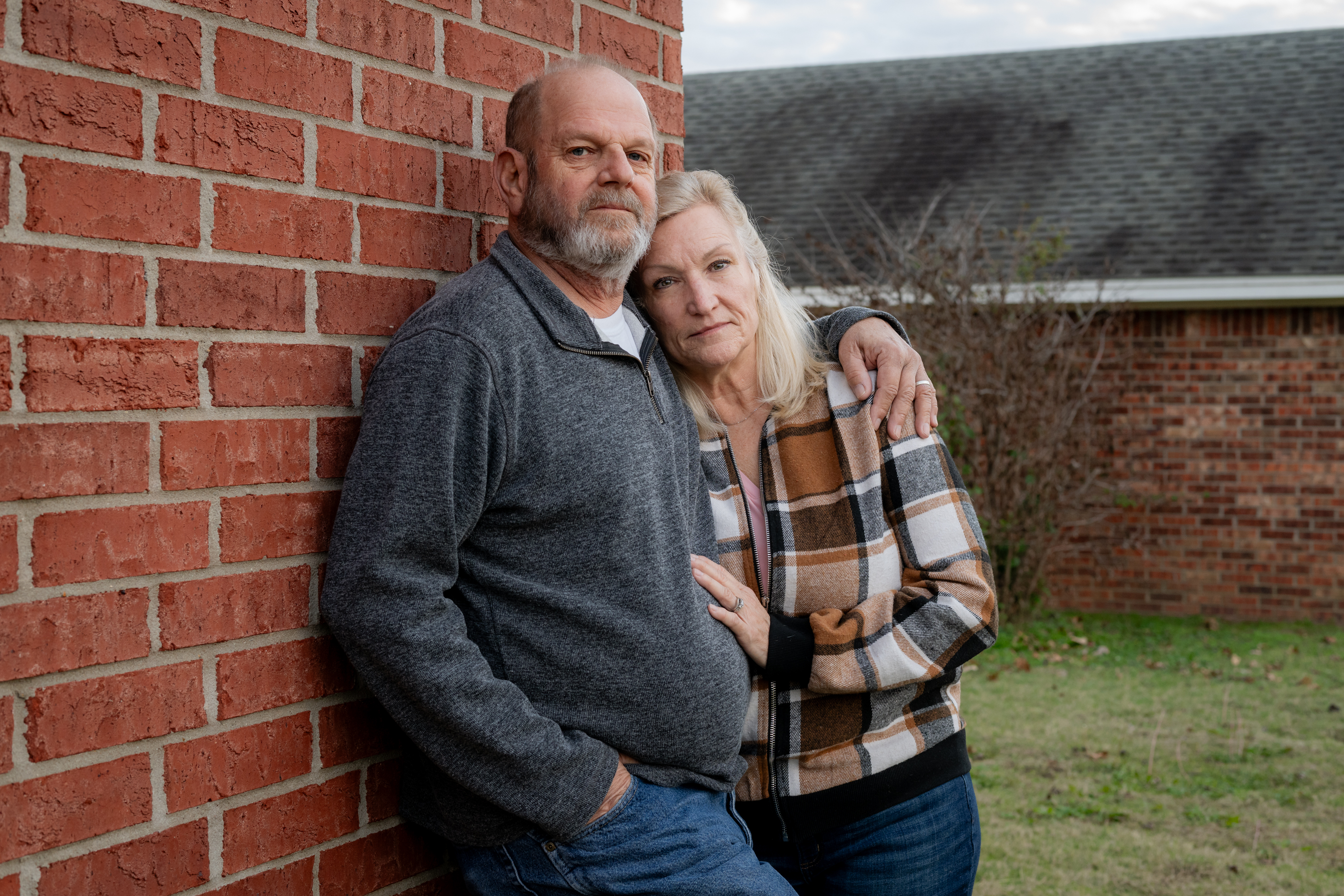
Marine Corps veteran Ron Winters clearly remembers his physician’s sobering evaluation of his bladder most cancers prognosis in August 2022.
“That is dangerous,” the 66-year-old Durant, Oklahoma, resident remembered his urologist saying. Winters braced for the battle of his life.
Little did he anticipate, nonetheless, that he wouldn’t be waging battle solely in opposition to most cancers. He additionally was up in opposition to the Division of Veterans Affairs, which Winters blames for dragging its ft and organising obstacles which have delayed his therapies.
Winters didn’t bear most cancers therapy at a VA facility. As an alternative, he sought care from a specialist via the Veterans Well being Administration’s Neighborhood Care Program, established in 2018 to boost veterans’ selections and scale back their wait instances. However he mentioned the prior authorization course of was a protracted nightmare.
“For them to take weeks — as much as months — to supply an authorization is ridiculous,” Winters mentioned. “It doesn’t matter if it’s most cancers or not.”
After his preliminary prognosis, Winters mentioned, he waited 4 weeks for the VA to approve the process that allowed his urologic oncologist on the College of Texas Southwestern Medical Heart in Dallas to take away among the most cancers. Then, when he completed chemotherapy in March, he was compelled to attend one other month whereas the VA thought-about approving surgical procedure to take away his bladder. Even routine imaging scans that Winters wants each 90 days to trace progress require preapproval.
In a written response, VA press secretary Terrence Hayes acknowledged {that a} “delay in care isn’t acceptable.” After KFF Well being Information inquired about Winters’ case, the VA started working with him to get his ongoing care licensed.
“We may also urgently overview this matter and take steps to make sure that it doesn’t occur once more,” Hayes instructed KFF Well being Information.
Prior authorization isn’t distinctive to the VA. Most personal and federal medical health insurance applications require sufferers to safe preapprovals for sure therapies, checks, or prescription medicines. The method is meant to cut back spending and keep away from pointless, ineffective, or duplicative care, though the diploma to which firms and companies set these guidelines varies.
Insurers argue prior authorization makes the U.S. well being care system extra environment friendly by slicing waste — theoretically a win for sufferers who could also be harmed by extreme or futile therapy. However critics say prior authorization has grow to be a instrument that insurers use to limit or delay costly care. It’s an particularly alarming difficulty for individuals recognized with most cancers, for whom immediate therapy can imply the distinction between life and dying.
“I’m fascinated with worth and affordability,” mentioned Fumiko Chino, a member of the Affordability Working Group for the Memorial Sloan Kettering Most cancers Heart. However the way in which prior authorization is used now permits insurers to implement “denial by delay,” she mentioned.
Most cancers is likely one of the most costly classes of illness to deal with within the U.S., in accordance with the Facilities for Illness Management and Prevention. And, in 2019, sufferers spent greater than $16 billion out-of-pocket on their most cancers therapy, a report by the Nationwide Most cancers Institute discovered.
To make issues worse, many most cancers sufferers have had oncology care delayed due to prior authorization hurdles, with some dealing with delays of greater than two weeks, in accordance with analysis Chino and colleagues revealed in JAMA in October. One other latest examine discovered that main insurers issued “pointless” preliminary denials in response to imaging requests, most frequently in endocrine and gastrointestinal most cancers circumstances.
The federal authorities is weighing new guidelines designed to enhance prior authorization for thousands and thousands of individuals coated by Medicare, Medicaid, and federal market plans. The reforms, if carried out, would shorten the interval insurers are permitted to contemplate prior authorization requests and would additionally require firms to supply extra info once they difficulty a denial.
Within the meantime, sufferers — a lot of whom are dealing with the worst prognosis of their lives — should navigate a system marked by roadblocks, crimson tape, and appeals.
“That is merciless and strange,” mentioned Chino, a radiation oncologist. A two-week delay may very well be lethal, and that it continues to occur is “unconscionable,” she mentioned.
Chino’s analysis has additionally proven that prior authorization is immediately associated to elevated anxiousness amongst most cancers sufferers, eroding their belief within the well being care system and losing each the supplier’s and the affected person’s time.
Leslie Fisk, 62, of New Smyrna Seaside, Florida, was recognized in 2021 with lung and mind most cancers. After seven rounds of chemotherapy final 12 months, her insurance coverage firm denied radiation therapy really helpful by her medical doctors, deeming it medically pointless.
“I keep in mind dropping my thoughts. I want this radiation for my lungs,” Fisk mentioned. After combating Florida Well being Care Plans’ denial “tooth and nail,” Fisk mentioned, the insurance coverage firm relented. The insurer didn’t reply to requests for remark.
Fisk known as the entire course of “horribly traumatic.”
“You need to navigate essentially the most sophisticated system on the planet,” she mentioned. “In the event you’re simply sitting there ready for them to deal with you, they gained’t.”
A new KFF report discovered that sufferers who’re coated by Medicaid seem like notably impacted by prior authorization, no matter their well being considerations. About 1 in 5 adults on Medicaid reported that their insurer had denied or delayed prior approval for a therapy, service, go to, or drug — double the speed of adults with Medicare.
“Shoppers with prior authorization issues are inclined to face different insurance coverage issues,” corresponding to bother discovering an in-network supplier or reaching the restrict on coated providers, the report famous. They’re additionally “much more more likely to expertise severe well being and monetary penalties in comparison with individuals whose issues didn’t contain prior authorization.”
In some circumstances, sufferers are pushing again.

In November, USA In the present day reported that Cigna admitted to creating an error when it denied protection to a 47-year-old Tennessee lady as she ready to bear a double-lung transplant to deal with lung most cancers. In Michigan, a former medical health insurance govt instructed ProPublica that the corporate had “crossed the road” in denying therapy for a person with lymphoma. And Blue Cross and Blue Protect of Louisiana “met its match” when the corporate denied a Texas trial lawyer’s most cancers therapy, ProPublica reported in November.
Numerous others have turned to social media to disgrace their medical health insurance firms into approving prior authorization requests. Laws has been launched in not less than 30 states — from California to North Carolina — to deal with the issue.
Again in Oklahoma, Ron Winters remains to be combating. In line with his spouse, Teresa, the surgeon mentioned if Ron might have undergone his operation sooner, they could have averted eradicating his bladder.
In some ways, his story echoes the nationwide VA scandal from practically a decade in the past, during which veterans throughout the nation had been languishing — some even dying — as they waited for care.
In 2014, for instance, CNN reported on veteran Thomas Breen, who was saved ready for months to be seen by a health care provider on the VA in Phoenix. He died of stage 4 bladder most cancers earlier than the appointment was scheduled.
Winters’ most cancers has unfold to his lungs. His prognosis has superior to stage 4.
“Actually, nothing has modified,” Teresa Winters mentioned. “The VA’s processes are nonetheless damaged.”
Do you may have an expertise with prior authorization you’d wish to share? Click on right here to inform your story.