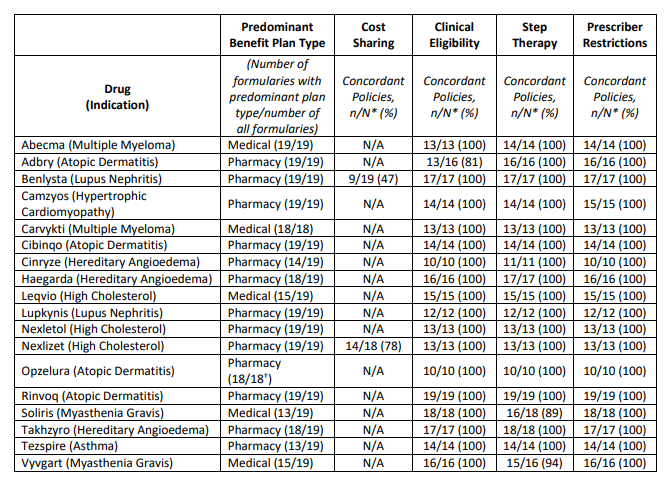
Final month, ICER launched their 2023 “Evaluation of Limitations to Honest Entry” . The report concludes the next relating to 18 medicine evaluated.
ICER defines “truthful entry” based mostly on the next standards:
Value sharing
- Value sharing based mostly on internet worth. Affected person value sharing must be based mostly on the web worth to the plan sponsor, not the unnegotiated record worth.
- No value for prime worth therapies. All drugs recognized by the Inner Income Service as high-value therapies ought to obtain pre-deductible protection inside excessive deductible well being plans.
- One low-cost possibility out there in every class. At the least one drug in each class must be lined on the lowest related cost-sharing stage except all medicine are priced greater than a longtime truthful worth threshold.
- Alright to have excessive value sharing if no medicine are cost-effective. If all medicine in a category are priced so that there’s not a single drug that represents a good worth as decided via worth evaluation, it’s cheap for payers to have all medicine on a better costsharing stage.
- If all medicine are priced at truthful worth, formulary placement is appropriate. If all medicine in a category are priced in order that they symbolize a good worth, it stays cheap for payers to make use of preferential formulary placement with tiered value sharing to assist obtain decrease total prices.
- Restricted cost-sharing if step-through required. As a part of financial step remedy, when sufferers strive a decrease value possibility with a decrease cost-sharing stage however don’t obtain an satisfactory medical response, value sharing for additional therapies also needs to be on the decrease cost-sharing stage so long as these additional therapies are priced pretty in keeping with clear standards.
Though ICER record six standards, solely three (#3, #4, and #5) are formally assessed of their report.
Scientific eligibility
- Payers ought to supply alternate options to prior authorization protocols corresponding to packages that give suggestions on prescribing patterns to clinicians or exempt them from prior authorization necessities (“gold carding”) in the event that they display excessive constancy to evidence-based prescribing.
- Payers ought to doc at the very least as soon as yearly that medical eligibility standards are based mostly on prime quality, up-to date proof, with enter from clinicians with expertise in the identical or comparable medical specialty.
- Scientific eligibility standards must be developed with express mechanisms that require payer employees to doc that they’ve: (i) thought-about limitations of proof as a result of systemic under-representation of minority populations; and (ii) sought enter from medical specialists on whether or not there are distinctive advantages and harms of therapy which will come up for organic, cultural, or social causes throughout completely different communities; and (iii) confirmed that medical eligibility standards haven’t gone past cheap use of medical trial inclusion/exclusion standards to interpret or slim the FDA label language in a method that disadvantages sufferers with underlying disabilities unrelated to the situation being handled
- For all medicine: Scientific eligibility standards that complement the FDA label language could also be used to: (i) set requirements for prognosis; and/or • Outline indeterminate medical phrases within the FDA label (e.g., “moderate-to-severe”) with express reference to medical tips or different requirements; and/or (ii) triage sufferers by medical acuity when the payer explicitly paperwork that triage is each cheap and essential
- For medicine with costs or worth will increase which were deemed cheap: Aside from the three functions outlined above, medical eligibility standards mustn’t deviate from the FDA label language in a fashion that would cut protection.
- For medicine with costs or worth will increase which were deemed cheap: Documentation that sufferers meet medical eligibility standards ought to symbolize a lightweight administrative burden, together with acceptance of clinician attestation in lieu of extra formal medical report documentation except documentation is important to make sure affected person security.
- For medicine with costs or worth will increase which were deemed unreasonable: Scientific eligibility standards could slim protection by making use of particular eligibility standards from the pivotal trials used to generate proof for FDA approval if applied with cheap flexibility and supported by strong appeals procedures as described within the implementation standards.
Step Remedy and Switching
- To be able to justify financial step remedy insurance policies extending past FDA labeling as applicable, payers ought to explicitly affirm or current proof to doc the entire following: • Use of the first-step remedy reduces total well being care spending, not simply drug spending
- The primary-step remedy is clinically applicable for all or almost all sufferers and doesn’t pose a larger danger of any vital facet impact or hurt.
- Sufferers may have an inexpensive probability to fulfill their medical objectives with first-step remedy.
- Failure of the first-step drug and the ensuing delay in starting the second-step agent is not going to result in long-term hurt for sufferers.
- Sufferers will not be required to retry a first-line drug with which they’ve beforehand had adversarial unintended effects or an insufficient response at an inexpensive dose and period.
- To be able to justify required switching insurance policies as applicable, payers ought to explicitly affirm or current proof to doc the entire following: (i) use of the required drug reduces total well being care spending. (ii) the required swap remedy is predicated on the identical mechanism of motion or presents a comparable danger and facet impact profile to the index remedy. (iii) the required swap remedy has the identical route of administration or the distinction in route of administration will create no vital destructive affect on sufferers as a result of medical or socio-economic elements. and (iv) sufferers will not be required to modify to a drug that they’ve used earlier than at an inexpensive dose and period with insufficient response and/or vital unintended effects, together with earlier use below a unique payer
Supplier {qualifications}
- Restrictions of protection to specialty prescribers are cheap with a number of of the next justifications: Ii) correct prognosis and prescription require specialist coaching, with the chance that non-specialist clinicians would prescribe the treatment for sufferers who could undergo hurt or be unlikely to profit. (ii) dedication of the dangers and advantages of therapy for particular person sufferers requires specialist coaching as a result of potential for severe unintended effects of remedy. (iii) dosing, monitoring for unintended effects, and total care coordination require specialist coaching to make sure secure and efficient use of the treatment.
- Requiring that non-specialist clinicians attest they’re caring for the affected person in session with a related specialist is an inexpensive possibility when the situation is regularly handled in main care settings however some parts of dosing, monitoring for unintended effects, and/or total coordination of care would profit from specialist enter for a lot of sufferers
Honest Entry Standards
- Value-sharing insurance policies must be introduced clearly to shoppers previous to well being plan choice, permitting all people to know what value sharing they’ll face for therapies they’re at present taking or are contemplating.
- Any vital change to formulary or value sharing constructions mustn’t happen mid-cycle except plan sponsors embody this as a qualifying occasion permitting plan enrollees to modify plans.
- On the level of care, clinicians and sufferers ought to be capable of quickly decide the cost-sharing necessities for any therapy together with value sharing for different alternate options.
- People contemplating well being plan enrollment must be introduced with clear info permitting them to know whether or not they meet the insurers’ medical standards for the therapies they’re at present taking. The insurance policies also needs to set out the rationale behind them and be readily comprehensible.
- Clinicians and sufferers ought to be capable of quickly decide the medical standards for any therapy and examine the medical rationale supporting these standards. The referenced medical info must be available to the prescribing/ordering supplier and the general public.
- People contemplating well being plan enrollment must be introduced with clear info permitting them to know whether or not the therapies they at present take or envision taking will probably be topic to non-medical step remedy or switching insurance policies.
- Clinicians, pharmacists, and sufferers ought to be capable of quickly decide the necessities associated to step remedy and switching insurance policies and be capable of simply view a full justification from the insurer.
- People contemplating well being plan enrollment ought to be capable of simply discover info associated to protection standards, together with prescriber {qualifications}, for medicine that they or members of the family are at present taking.
- Clinicians and sufferers ought to be capable of quickly decide whether or not there’s a restriction on prescribing for any therapy. Insurers ought to present prepared help to main care clinicians searching for reference to a related specialist for session as wanted
You may learn the total report right here.